The Scleral Contact Lens
The scleral contact lens can improve vision in many advanced refractive disorders including keratoconus which is the focus of this article.
Advancement in technologies behind the scleral contact lens makes it one of the preferred options by ophthalmologists and clients. Here we will discuss:
- Advancement in scleral contact lens technology.
- Evolution of the scleral contact lens.
- How the scleral lens is fabricated.
- My experience with the scleral contact lens.
Advancement
The advancement in materials leads to better customization and increased comfort.
Advancement of the scleral contact lens in the areas of comfort and customization makes the scleral contact lens an excellent option to restore vision in the above-mention scenario.
With many more manufacturers producing the scleral lens, in addition to better technology, the scleral contact lens is highly customizable to better fit the needs of each individual case.
These factors make the scleral contact lens an excellent option among patients and practitioners to help restore vision for those of us dealing with irregular astigmatism and advanced refractive errors.
In addition to improvements in manufacturing process of the scleral contact lens, likewise has the ability to customize the lens improved. Both advancements work in tandem to help increase quality of life.
Customization
Improved customization provides better comfort for those of us that rely on the lens to function daily. For many years, one of the major drawbacks of any lens was comfort.
In other words, the lens can be manufactured from the best materials. However, if comfort is an issue, wearing the lens, even for a short amount of time can be troublesome and impossible for some, thus keeping the dropout rate high.
To put it differently, one of the difficulties for the practitioner is to acquire a proper fit for those of us with advanced refractive errors like keratoconus.
Advancements in technology now allows the practitioner to map the cornea more precisely. Coupled with the manufacturer’s ability to take that raw data and apply it to fabricate a lens to the practitioner’s exact parameters.
It is one of the factors that makes the scleral contact lens an option worth looking into.
Evolution of the Scleral Contact Lens
To understand how the materials and fabrication process has improved we must first look to the past.
We won’t go back to 1880’s when the first lens was fabricated from blown glass. Rather we can begin when the lens was made from polymethylmethacrylate (PMMA).
This material in terms of durability, optical quality, and ease of care was reliable. However, there was one drawback. The PMMA has an oxygen transmissibility of 0.
Not only is fit and comfort an area of importance, additionally, so too is the oxygen transmissibility of the lens.
In other words, how much oxygen does the lens allow to reach our cornea. A Lack of oxygen to the cornea can lead to severe complications.
Adding Silicone
The addition of silicone was the next evolution in the scleral contact lens. With the addition of silicone, oxygen was now able to pass through the lens instead of around the lens.
Having said that, today this material is much less common due to increased wettability issues, surface deposits and comfort issues.
Adding Fluorine
Moreover, another major advancement in the scleral contact lens was the addition of fluorine which brings us to the present-day lens.
The addition of fluorine lowered surface tension, decreased the attraction of polarized tear components to the lens and reduced the incidence of ocular dryness.
Surface Treatments
The types of surface treatments to the scleral contact lens we will touch on are Plasma and Tangible Hydra-PEG which is now becoming much more of the standard in high end GP lens care.
Plasma
The plasma surface treatment improves the lenses materials wettability and the lenses interaction with the tear film.
In short, the plasma treatment ionizes the lens, therefore allowing the lens to be more hydrophilic. In other words, it increases the ability of the scleral contact lens to stay moist.
Furthermore, the treatment allows the lens to better deal with protein deposits, bacteria and contaminants better.
On the other hand, it is important to note that the ionization does not last forever and can be reduced with the use of abrasive cleaners.
Hydra-PEG
The Hydra-PEG add-on treatment is rapidly taking the place of the plasma treatment which was the standard surface treatment 10-15 years ago.
What is Hydra-PEG
Hydra-PEG is 90% water, and the rest is polyethylenethgycol or PEG. It is a common component of many artificial tears that also has a history in wound care management. The coating increases lubricity and comfort which can lower patient drop out rate.
How Does it Work
Firstly, the lens must be prepared by either adding a functional activator to the mix or to add a short plasma treatment. Once either one of the before mentioned additions has been added, the lens is then soaked in Hydra-PEG during the extraction/hydration process.
Hydra-PEG permanently bonds to the surface of the lens. This process will optimize the surface’s wettability, lubricity, tear stability and resistance to deposits.
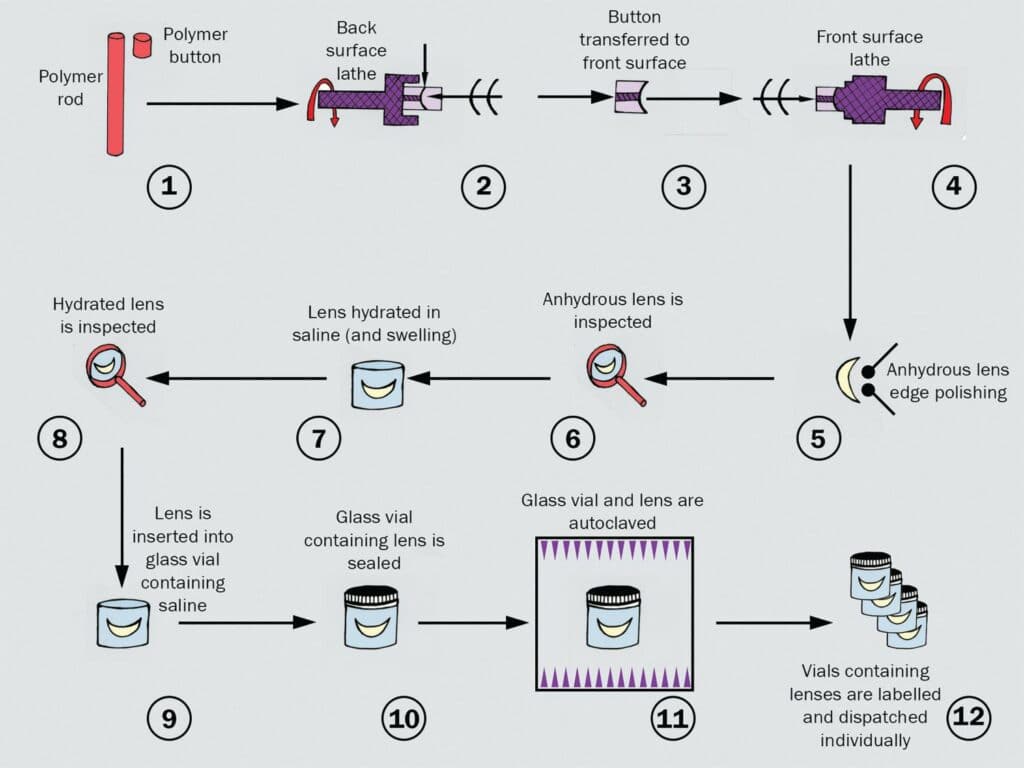
Fabrication
How is the scleral contact lens fabricated? Data from our ophthalmologist which determines the prescription, diameter and mapping parameters will be sent to the manufacturer.
This data will be entered into software and will be used during the manufacturing process.
Molding Method
The molding of the lens can be done several different ways.
Spin cast
Developed in Prague, the spin cast method involves three different fluids poured into rotating molds. The outside curvature of the lens is shaped by the mold itself; however, the inside was formed according to the speed of the rotation of the mold.
The centrifugal force of the spinning mold leads to the polymerization of the fluids linking the molecular chains to form the required hydrophilic plastic.
Injection
Injection molding involves injecting molten plastic under pressure into the mold. The lens is finished on a lathe although it is now possible to manufacture the lens entirely through molding that does require lathe cutting.
This can be achieved thanks to the advancement in automated computer-controlled mold production technology.
Lathe Method
The initial forming of the lens can also be done by cutting on a lathe.
Firstly, a blank is made. The blank is a circle slightly larger than the finished product. This can be cut from a plastic rod or stamped from a plastic sheet. The blank is fastened to a steel button with a drop of molten wax.
Second, the button is then centred on the lathe which in turn spins at high rpm. A cutting tool is used which can be diamond or laser. Indicators on the lathe measure the depth of the cuts to guide the lens operator
The button, securing the blank, as mentioned earlier, is moved to a lapping machine. The lapping machine holds the blank against the lapper which is a spinning disk coated with an abrasive compound. The shape of the lapper matches that of the lens.
The lapping machine spins the blank in one direction and the lapper in another. Furthermore, the blank also moves in small figure eight direction polishing the lens surface.
The polished lens is then mounted on a steel shaft called an arbor. The arbor has been ground to match the shape of the lens to ensure the lens fits on the arbor.
The arbor is installed on the lathe and the technician makes convex cuts to form the other major curve. This side of the lens is now polished, and the lapper is modified to fit the other side of the lens.
Once the second side is polished the lens is now considered semi-finished.
Finishing
The lens will require several more curves to be ground before the lens can be considered wearable.
The Future
As mentioned earlier, the materials that are used to fabricate the scleral contact lens continue to evolve tremendously since the first lens was created.
Equally important, is the advancement in the technology that allows the practitioner to set the parameters that are sent to the manufacturer to customize each lens during the manufacturing process.
To Summerize

The choice to opt for the scleral contact lens will be up to you and your practitioner. However, with the rapid advancement in technology in the fields of AI, robotics and cybernetics.
The scleral contact lens will only continue to be improved on providing a better fit, better customization and improved vision equalling better quality of life.
If you haven’t explored the scleral contact lens and are suffering from advanced refractive errors like keratoconus, this option might be something you and your practitioner might consider.
Here is another great resource from Review of Optometry on this same subject. Please have a look here.
My Experience with the Scleral Contact Lens
As with many of you, my story with a refractive error, keratoconus in my case, lead to me eventually needing a cornea transplant in my right eye.
After some time, glasses were no longer of much help to me. I had difficulties performing basic activities and couldn’t function at an average level outside of my home.
I tried rigid gas permeable lenses. The comfort level was so low that I was unable to continue wearing them. The scleral contact lens was a life changer for me.
My vision is 20/20 with the scleral contact lens. For myself, comfort is no longer an issue. I can wear them 10hrs to 13hrs at a time.
It’s important to note that results may vary from person to person. My results may differ from yours.
Discover More About Keratoconus
Don’t stop your journey here! For more in-depth information and the latest research on living with keratoconus, click here. Dive into a world of knowledge and resources that can empower you in managing keratoconus effectively.
Your vision for a clearer future starts with one click.